Student “Hot Spotters” Help Improve Lives for Complex Patients
Sophia Fong learned a lot about healthcare from Patient A.
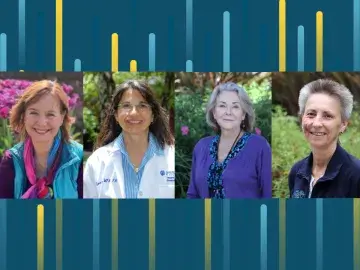
Fong, a physical therapy student at Samuel Merritt University (SMU), signed up as a volunteer in the pilot “Hot Spotting” program in July to work with patients known as 
Along with three other SMU students, Fong made house calls and met with the patients outside the hospital to assist with their daily needs in an effort to improve the patient’s quality of life and, ultimately, keep the clients from re-entering the ER.
One of the patients, referred to by the students as Patient A, was a prostitute and drug addict. By talking to her and learning the details of her life, Fong said she came to understand the difference between prescribing healthcare remedies and empathizing with patients.
“I learned that we can provide medicine or exercise to our clients to make them feel better,” Fong said. “But that’s not the same as providing care. I found that if I just listened, and if that patient felt like she was being heard, that alone can be better than giving someone a pill.”
Fong talked about her volunteer service as part of the Complex Care Community Forum with Dr. Jeffrey Brenner at SMU’s Oakland campus on Nov. 3.
Brenner, a MacArthur “Genius” Fellow and executive director of the Camden Coalition of Healthcare Providers, is a nationally renowned physician who coined the term “hot spotting” to describe the strategic use of data to locate and serve high-utilizing patients.
He was profiled in the New Yorker and by PBS Frontline for his innovative work to improve care for complex patients.

“The most subversive thing in America today are these four students,” Brenner told the audience. “They would cut costs and close hospitals. And we should cheer every time a hospital closes.”
Brenner’s Camden Coalition developed a training and curriculum for student hot spotters at healthcare universities across the nation. The SMU team, joined by a medical student from UC Berkeley, is the first cohort from the East Bay.
“This is an opportunity to train the next generation of healthcare providers,” said Jim Hickman, CEO of Sutter Health’s philanthropic foundation Better Health East Bay, which sponsored the SMU students. “We’ve spent a lot of time in healthcare fitting people into the system. Now we have models and data to fit systems to the people.”
Maggie Balma, an SMU hot-spotter who will graduate from the nursing program next month, said she was surprised to learn how complicated and inaccessible the healthcare system appears to a complex care patient even after they leave the hospital. A deluge of appointments and obstacles make it appear overwhelming.
She said in her clinical rotations she spent 15 to 30 minutes talking to a patient about their lives.
With Patient A, she spent hours over several weeks to get a full picture.
“I’m grateful for what I learned from her,” Balma said.
She added that she wished the experience was required for first-year students entering SMU.
“Putting hot-spotting into the curriculum would make us all better providers,” Balma said. “We’d get a better understanding of all the barriers the patients encounter.”