Welcome to the Function in Sitting Test (FIST) Web-based Training
This website will train rehabilitation and medical professionals on how to administer a standardized test of sitting balance, the Function In Sitting Test or FIST, intended to be used in patients/clients who are suspected of having problems with balance and/or safety in a seated position. Thank you to the Department of Physical Therapy and Information Technology Services at SMU for hosting this training on their website.
This online module consists of an overview of the FIST, specifics related to each of the 14 FIST items, and documentation information. All FIST items have video examples showing different levels of performance. There is a brief quiz to assess competency available after you complete this tutorial.
First, some general information about the FIST.
What is the FIST?
- Useful: The FIST is a clinical examination of sitting balance, designed to be conducted at the patient's bedside
- Practical: Consists of 14 functional, everyday activities as test items
- Easy: Performance is scored by therapist using a single set of scoring criteria for all 14 items
- Quick: Most patients can easily complete the FIST in under 10 minutes
Purposes of the FIST
The FIST can be useful for a variety of clinical uses including:
- Assess functional sitting abilities
- Describe sitting balance dysfunction
- Focus interventions
- Track changes in sitting balance over time
- Assessment of lower level patients, especially if other balance tests may be too difficult for the patient
Is my patient appropriate for testing with the FIST?
The FIST is best suited for patients with:
- The ability to follow simple directions, either verbal or nonverbal
- Known or suspected sitting balance deficits
- Impulsiveness
- Safety issues in sitting
- Slow movement
- Poor seated motor control
- Lower level patients who...
- cannot tolerate other balance tests
- are unable to stand or ambulate without excessive assistance or devices
Patients who may benefit from other types of balance testing include:
- Patients who can...
- stand or perform more complex ADLs
- ambulate
- Patients who aren't yet...
- medically stable for sitting
- cleared for the motions or tasks on the FIST
Creation of the FIST
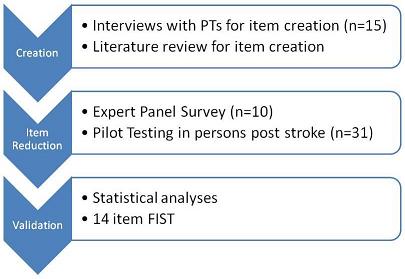
Please see the paper published in the Journal of Neurologic Physical Therapy detailing the development and validation of the FIST for more details, or view the abstract at PubMed.
Psychometrics of the FIST
- FIST reliability & validity summary
- Functional sitting balance ability explains 83.33% of score variance between persons
- Cronbach's alpha = 0.98
- In nonambulatory persons with MS = 0.91
- Person separation reliability = 0.978
- Standard error of measurement = 1.40
- Minimal detectable change (95% confidence) = 5.5 points
- Test-retest reliability (ICC, 95% confidence) = 0.97
- In nonambulatory persons with MS (ICC, 95% confidence) = 0.92
- Inter-tester and intra-tester reliability (ICC 95% confidence) = 0.99
- Standardized response mean = 1.04
- Index of responsiveness = 1.07
- Effect size = 0.83
- Concurrent validity with FIM and Berg Balance Scale at inpatient rehab admission (r=0.71 to 0.85)
- Minimal clinically important difference during inpatient rehab was change in FIST greater than 6.5 points
- FIST cutoff score indicating higher likelihood of discharge NOT to home (with or without assistance) measured within first 5 days of inpatient rehabilitation < 42 points.
- FIST significantly correlated with virtual time to contact in sitting in nonambulatory persons with MS (spearman's rho = 0.487, p = 0.02)
- See the References sectionfor studies and publications associated with the above listed reliability & validity results.
- Studies to determine evaluative validity in other applicable patient populations, predictive validity, and fall risk are underway and/or in planning stages. See our Research Collaboration page if you would like to participate in current/upcoming studies.
The FIST was designed as a bedside clinical measure, so the required equipment is simple and readily available in clinics and hospitals.
Equipment for FIST testing:
- Stopwatch, or watch with second hand--to time 30 seconds of performance (2 items)
- Tape measure--to measure 2 inches required to scoot (3 items), and to use as a lightweight object for patient to pick up (2 items)
You may also need:
- Small lightweight object, if not using the tape measure. A pen or cone could be used.
- Stool or step to position the patient's lower extremities depending on patient height and bed height.
- Chair for therapist positioning.
Position the patient:
Before having the patient perform any of the 14 items on the FIST, they should be positioned in the standard starting position. The therapist may help the patient and reposition them between items as needed.
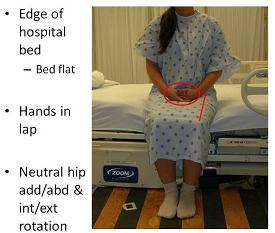
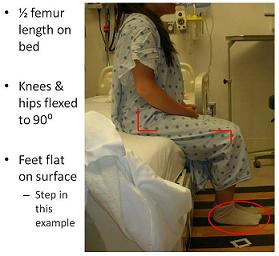
Note the patient is on a normal hospital bed without a mattress overlay and the bed is fully flattened. The patient's feet are flat on the floor, with the hips and knees at approximately 90 degrees of flexion. You should use a step or stool to position the lower extremities and feet if the patient is shorter. The hips are positioned so that hip rotation is neutral and they are not in hip abduction or adduction. The patient's hands are in the lap.
Position yourself:
Therapist positioning is determined by patient safety requirements to guard the patient appropriately and to allow the therapist to provide physical assistance to the patient should they need it during testing. Common positions for the therapist include sitting in front of the patient or to the side of the patient. The therapist can move between these positions as needed during testing.
Describe the FIST to the patient:
It is important that prior to beginning testing you describe the FIST to the patient. Not only does this help confirm informed consent for testing with the FIST, but it allows the patient to better understand what you will be doing and why. It also allows you to review some of the general principles of the FIST and FIST scoring prior to starting the FIST. You may choose to read the following prepared description to your patients:
"I will be conducting a test with you today to see how well you balance yourself in a sitting position. It will involve you sitting with your best posture and balance, as well as moving in a seated position to reach and scoot. I might lightly push you to see how well your balance reactions work. I will be right here next to you to make sure you are safe if you lose your balance. I would prefer if you could perform the test without using your hands for balance, but if you need to use your hands, you can. I will remind you to try to not use your hands during the test. If you need a break, just let me know and we can pause to let you rest. Do you have any questions? [Pause, answer questions] Let's start."
If you choose the paraphrase the directions for the FIST, be sure you include the following points:
- The FIST tests balance in seated position
- The patient should perform items with their best posture and balance, and while moving in a seated position
- The therapist will give them occasional light pushes to test for balance reactions
- The therapist will make sure they won't lose their balance
- The patient should try not to use their hands, but they can if they must
- The therapist will remind the patient to try to not use their hands
- Breaks are allowed-if the patient needs one, they should tell the therapist
- The therapist should ask the patient if they have questions, and answer them before proceeding
Now you should be able to set up FIST testing, including what equipment is required, patient positioning, therapist positioning, and general FIST description to use when testing.
The scoring criteria on the FIST are the same for each item. The FIST was designed this way to make learning and using the scoring scale easy and to decrease the need to constantly refer to written directions when scoring each item. The items are scored on a 5 point ordinal scale ranging from 0 to 4, with 0 representing the lowest ability and 4 representing normal ability.
0 Dependent
1 Needs assistance
2 Upper extremity support
3 Verbal cues/increased time
4 Independent
Let's take a look at each point on the scale.
0 Dependent: Patient requires complete physical assistance to perform task successfully, patient is unable to complete task successfully even with physical assistance, or dependent
- Without complete assistance, cannot complete the task successfully or safely
1 Physical Assistance: Patient is unable to complete task successfully without physical assistance
- Cannot complete the task safely or completely without physical assistance of the therapist
- Documentation of level of physical assistance needed by the patient is also required for this score
- minimal assistance or min A (25% or less effort provided by therapist)
- moderate assistance or mod A (26-74% of the effort provided by the therapist)
- maximal assistance or max A (75% or more of the effort provided by the therapist)
2 Upper Extremity Support: If the patient requires the use of one or both of their upper extremities to support themselves or to maintain their balance during the performance of the task, they score a 2. Items involving grasping or picking up items should be scored a 2 if the patient uses their upper extremity for support or balance, not as a score of how they pick up the item. Items that involve a movement and require the patient return to the starting position should be scored a 2 if the patient requires the use of their hands for any part of the task. You may prompt the patient to try again without using their hands to see if they are able to successfully complete the task without their hands.
- Must use hands for successful completion of task or to maintain balance during task
3 Verbal Cues/ Increased Time: A score of 3 indicates the patient required verbal cueing or an increased amount of time to complete the task. Otherwise, their performance was complete and they successfully completed the task. If a patient is unsafe but can otherwise complete the task, and providing verbal cueing would improve safety (i.e.,"slow down"), the patient is scored as a 3.
- Performance is normal but cues are needed or longer than normal time is needed
4 Independent: 4 is the highest score attainable for any individual item and represents performance that is normal. It also accounts for speed and safety.
- Reaction and performance you would expect as normal
- Speed and safety also normal
Now you should be familiar with the scoring scale used for all the FIST items.
Read more about the FIST item overview.
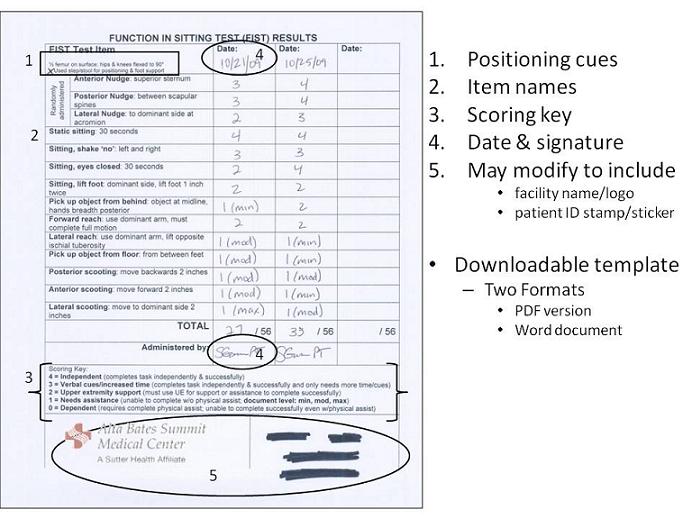
Ensure accurate reporting of your patient's FIST results using the following:
Paper documentation: Templates are available for downloading to use in your facility/clinic.
Modification to include facility name/logo and patient ID stamp/sticker is acceptable. Otherwise, please do not modify these templates without express written permission of the author.
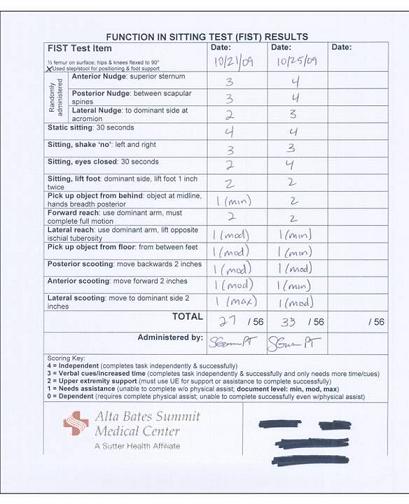
Here is an example of a completed documentation form.
Note the following aspects of this form, as described below.
Electronic Health Record (EHR) documentation:
The FIST can be imported into EHR systems. It is suggested that the brief descriptors of each item be included as a prompt for correct performance and documentation, and that scores be accessed via a drop down menu if possible. Please follow the same templates when converting to EHR as much as possible, and do not significantly alter the documentation template when converting to EHR without the express written consent of the author.
- Example of formatting of FIST embedded into EHR (courtesy of Connie Marsh Bartle, PT, DPT, CEEAA)
Patients may change in 3 distinct ways, as shown in this example.
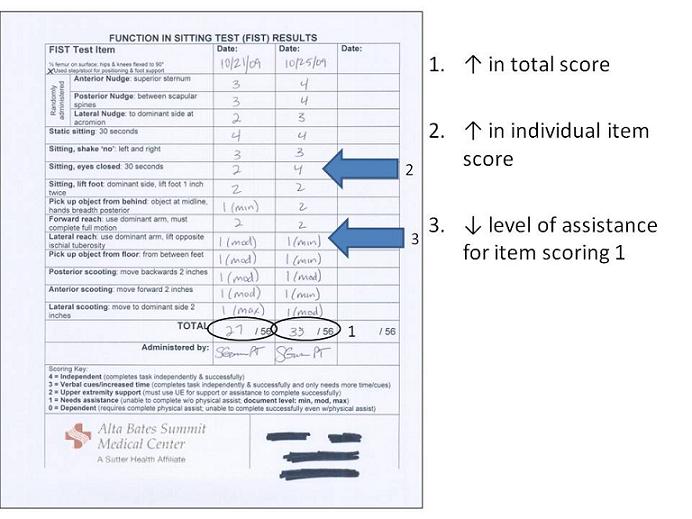
- They may increase their total score, as seen in this example with a rise from 27 to 33.
- They may also increase their score on individual items, as seen here the patient now can sit with their eyes closed independently.
- The level of physical assistance required to safely, completely, and successfully complete an item may change for an item still scoring a 1. In this example, the patient now only requires minimal assistance to perform the lateral reach item.
The minimal detectable change (change that exceeds error) is a change greater than 5 points.The minimal clinically important difference during inpatient rehabilitation is a change greater than 6 points. (see References for details)
Now you have covered the entire FIST and should be ready to begin testing using the FIST.
When administering the FIST, remember...
- FIST overall description
- Give your patient the general description of the test at the start.
- Patient position
- Correct the patient's position and reposition as needed before moving onto the next item.
- Examiner position
- Position yourself to ensure patient safety and allow you to assist as the patient as needed.
- Item directions
- Describe and demonstrate each test item before scoring the patient's performance.
- Scoring criteria
- 0 to 4 score for each item
- Record physical assistance level if scoring item as 1
- min, mod, or max A
The following written resources are available for you to download.
- FIST Training Manual (pdf), version 1.5
- Documentation templates
You've completed training in the administration of the FIST. Congratulations!
FIST Post-Training Quiz
This is a 10 question test.
- 4 questions use video clips to assess your ability to assign a FIST score based on patient performance of specific FIST items.
- Videos will play twice.
- 6 multiple choice questions assessing your knowledge of set up, patient directions, FIST items, documentation, and other aspects covered during this web-based training.
Directions: Please select the BEST answer. Click this link to launch the quiz.
The Function In Sitting Test (FIST) was created to allow healthcare providers to better describe patient abilities to move and perform functional tasks in sitting. Administration of the FIST was intended for persons who are cleared for sitting and do not have any contraindications for moving in the prescribed manner for the individual test items. Determination of a patient's ability to safely perform the FIST lies solely with the healthcare provider administering the FIST. Additionally, as a test of balance in a seated position, it is the healthcare provider's responsibility to guard and supervise the patient at all times during the administration of the FIST to prevent falls or other unwanted or unexpected outcomes.
FIST references
Alzyoud J, Medley A, Thompson M, Csiza L. Responsiveness, minimal detectable change, and minimal clinically important difference of the sitting balance scale and function in sitting test in people with stroke. Physiother Theory Pract. 2022;38(2):327-336. doi:10.1080/09593985.2020.1756016 [View abstract online]
Palermo AE, Cahalin LP, Garcia KL, Nash MS. Psychometric Testing and Clinical Utility of a Modified Version of the Function in Sitting Test for Individuals With Chronic Spinal Cord Injury. Arch Phys Med Rehabil. 2020;101(11):1961-1972. doi:10.1016/j.apmr.2020.06.014 [View abstract online]
Cabanas-Valdés R, Bagur-Calafat C, CaballeroGómez FM, et al. Validation and reliability of the Spanish version of the Function in Sitting Test (S-FIST) to assess sitting balance in subacute post-stroke adult patients.Topics Stroke Rehabil, 2017; e-pub April 13, 2017. DOI:10.1080/10749357.2017.1316548 [View the abstract online]
Sung JH, Ousley CM, Shen S, Isaacs ZJK, Sosnoff JJ, Rice LA. Reliability and validity of the function in sitting test in nonambulatory individuals with multiple sclerosis. Int J Rehabil Res. 2016;39(4):308-312.[View the abstract online]
Gorman S, Harro C. Function In Sitting Test admission score predicts inpatient rehabilitation discharge destination.. Poster Presentation. IV STEP Conference, American Physical Therapy Association, Columbus, OH, July 17, 2016. [View the abstract online]
Gorman SL, Harro C, Platko C, Greenwald C. Examining the Function In Sitting Test (FIST) for validity, responsiveness, and minimal clinically important difference. J Arch Phys Med Rehabil. 2014;95(12):2304–2311. [View the abstract on PubMed]
Ousley CM, Isaac ZJK, Wajda DA, Rice LA, Sosnoff JJ. Validation of seated postural control measures in persons with multiple sclerosis. (poster) 4th International Symposium of Gait and Balance in Multiple Sclerosis. Cleveland, Ohio, Oct 10-11, 2014.
Gorman SL, Rivera M, McCarthy L. Reliability of the Function In Sitting Test (FIST). Rehabil Res Prac. 2014;Article ID 593280,http://dx.doi.org/10.1155/2014/593280. [View the open access article here]
Mustille R, Petersen H, Abele J, et al. A pilot study of the FIST as a functional outcomes measure in a neurological acute care population (abstract). J Acute Care Phys Ther. 2013;4(3):129-130. [View the abstract here]
Rideout D, Nordstrom TM, Lazaro RT. Case 6: Coccidioidomycosis meningitis. In: Jobst E, ed. Case Files in Physical Therapy (Neurological Rehabilitation). Boston, MA:McGraw-Hill; 2014.
Gorman SL, Harro C, Platko C. Validity and responsiveness of the Function In Sitting Test (FIST) in adults in inpatient rehabilitation: preliminary results (abstract). J Rehabil Med. 2013;6(Suppl 53):99. [View the conference proceedings open access]
Gorman SL. Case 1: Acute cerebrovascular accident. In: Jobst E, ed. Case Files in Physical Therapy (Acute Care). Boston, MA:McGraw-Hill; 2013.
Gorman SL, Radtka S, Melnick M, Abrams G, Byl NN. Development and validation of the Function In Sitting Test (FIST) in adults with acute stroke. J Neuro Phys Ther. 2010:34(3);150-160. [View the abstract on PubMed]
How to cite this web-based training (AMA 11th edition):
Gorman SL. Function In Sitting Test Web-Based Training. Samuel Merritt University website. https://www.samuelmerritt.edu/fist. Published June 2011. Updated May 2023. Accessed [insert date].
Thank you to the many people who helped during the development of the FIST and with this web-based training:
- UCSF/SFSU DPTSc Program Faculty & Students
- UCSF Department of Physical Medicine & Rehabilitation Science
- California Physical Therapy Association and the Cal PT Fund for their grant support
- Please consider making a donation to support physical therapy research in California through the Cal PT Fund.
- Clinicians at UCSF Medical Center for their assistance in participant recruitment
- Samuel Merritt University Department of Physical Therapy & IT Department
- Clients/patients who participated in the validation studies of the FIST
- Clients, patients, and therapists who agreed to be featured in photos and/or videos used in this training
There is a modified version of the FIST for use in persons with spinal cord injury. View the abstract here.
The FIST is available in the following translations:
- French (translation courtesy of Sonia Nguyen, physiotherapist at IRGLM, Montreal, Canada)
This version has yet to be validated via study. - Spanish (translation courtesy of Rosa Cabanas-Valdés, Departament de Fisioterapia, Facultat de Medicina i Ciencies de la Salut, Universitat Internacional de Catalunya, Barcelona, Spain. She was assisted by Raúl Moya Valdés, Occupational Therapist, Licenciado en Ciencias de la Ocupación, Universidad de Chile, Chile) Dr. Cabanas-Valdés is the lead author of a study validating the Spanish FIST for reliability, validity, and responsiveness. View the abstract here.
- Turkish (translation courtesy of Büşra Nur Erol, Saniye Aydoğan Arslan, Evren Yaşar, Esra Dilek Keskin, Cevher Savcun Demirci) Dr. Erol is the lead author of the reliability and validity of the Turkish FIST in persons with stroke. View the abstract here.
Other translations of the FIST are underway:
- Japanese
- Portuguese
- Hebrew
- Mandarin
If you would like to work on an underway translation or volunteer to translate the FIST into another language, please contact us for more information.
If you still have questions about FIST administration or scoring, or would like to work on a translation of the FIST, please contact the creator, Sharon Gorman, PT, DPTSc, GCS, FNAP.
email: sgorman@samuelmerritt.edu
There is an active research agenda underway involving the FIST. The following projects are currently in progress. If your facility would like more information on potential research collaborations, please get in touch with the contact person listed below.
- Relationship of the FIST to gait and transfer ability recovery
- This study is in the planning stages, please contact Dr. Sharon Gorman
- Determination of FIST cut-off score for fall risk determination
- This will most likely be a multi-center study looking at the relationship of FIST scores and established fall risk tools to determine if a FIST cut-off score for fall risk can be described. Population of interest will most likely be hospital or skilled nursing based.
If you or your facility would like to collaborate on another project using the FIST, please contact us to discuss future opportunities and collaborations.
[updated 5/25/23]
Function In Sitting Test © 2009 by Sharon L. Gorman, PT, DPTSc is licensed underCC BY-ND 4.0